Symptom analysis is a crucial process in healthcare that helps identify underlying health conditions based on a patient’s reported experiences. By evaluating the type, duration, severity, and pattern of symptoms, healthcare professionals can narrow down possible diagnoses and initiate appropriate treatment.
Table of Contents
- What Is Symptom Analysis?
- Why Symptom Analysis Is Important
- The Process of Symptom Analysis
- Common Symptom Categories
- Tools and Technologies in Symptom Analysis
- Role of AI in Symptom Analysis
- How to Perform a Self Symptom Analysis Safely
- Symptom Patterns Across Common Diseases
- Symptom Analysis vs. Diagnosis
- Symptom Tracking and Journaling
- Case Study: Symptom Analysis in Chronic Illness
- User Behavior and Bias in Symptom Reporting
- Future Trends in Symptom Analysis
- Conclusion: Empowering Health Through Symptom Awareness
What Is Symptom Analysis?
Symptom analysis refers to the detailed examination and interpretation of symptoms reported by an individual. These symptoms are subjective experiences such as pain, fatigue, dizziness, or nausea. Unlike signs, which are measurable indicators (like blood pressure or temperature), the patient feels and expresses symptoms.
Healthcare providers use symptom analysis as a critical first step in clinical reasoning. Combining symptom data with medical history, examination findings, and lab tests, they build a differential diagnosis — a list of possible conditions that could be causing the issue.
Why Symptom Analysis Is Important
Understanding symptoms properly can lead to early detection of diseases, which is essential for effective treatment. Many chronic conditions, including diabetes and cardiovascular disease, begin with subtle symptoms that are often ignored.
Benefits of Accurate Symptom Analysis
- Timely treatment: Enables quicker identification and intervention.
- Reduction in diagnostic errors: Prevents misdiagnosis or delayed diagnosis.
- Lower healthcare costs: Avoids unnecessary procedures and hospitalizations.
- Better patient outcomes: Leads to personalized, targeted care.
- Patient empowerment: Encourages individuals to be proactive in health monitoring.
Consider someone with persistent fatigue — this could indicate anemia, thyroid issues, sleep apnea, or even depression. Without symptom analysis, the true cause may remain hidden for months.
The Process of Symptom Analysis
Doctors use structured frameworks to assess symptoms thoroughly. The most common is the OPQRST method:
Key Elements of Symptom Analysis
| Element | Description |
| Onset | When did the symptom begin? Sudden or gradual? |
| Provocation/Palliation | What worsens or improves the symptom? |
| Quality | What does the symptom feel like? Sharp, dull, burning, etc. |
| Region/Radiation | Where is the symptom located? Does it spread? |
| Severity | How intense is the symptom on a scale of 1–10? |
| Time/Duration | How long does it last? Is it constant or intermittent? |
Case Example
A 52-year-old man reports chest pain. Using OPQRST:
- Onset: Began during exercise
- Provocation: Worse with exertion, relieved by rest
- Quality: Pressure-like, not sharp
- Region: Central chest, radiates to the left arm
- Severity: 7/10
- Time: Lasts around 10 minutes
These findings point strongly toward angina, warranting further cardiac evaluation.
Common Symptom Categories
Grouping symptoms into categories helps in recognizing patterns and narrowing down possible conditions. Below are common categories and examples:
| Category | Examples |
| Neurological | Headaches, dizziness, numbness |
| Cardiovascular | Chest pain, palpitations, shortness of breath |
| Gastrointestinal | Nausea, vomiting, abdominal pain |
| Respiratory | Cough, wheezing, chest tightness |
| Musculoskeletal | Joint pain, stiffness, swelling |
| Dermatological | Rashes, itching, discoloration |
| Psychological | Anxiety, mood swings, insomnia |
| Endocrine | Fatigue, weight changes, heat/cold intolerance |
Each of these symptom groups can point to vastly different conditions, depending on associated factors.
Tools and Technologies in Symptom Analysis
Advancements in digital health have revolutionized how we analyze symptoms.
Modern Symptom Analysis Tools
- Symptom Checker Apps: Tools like WebMD, Ada, and Isabel help users assess symptoms interactively.
- Electronic Health Records (EHRs): Track symptoms over time, allowing longitudinal analysis.
- Remote Monitoring Devices: Smartwatches and fitness trackers monitor heart rate, oxygen saturation, and sleep quality.
- Telemedicine Platforms: Enable symptom evaluation without visiting a clinic.
Limitations to Keep in Mind
- Accuracy depends on user input
- May miss nuances like emotional tone
- Cannot replace physical examinations
Role of AI in Symptom Analysis
AI is significantly enhancing the accuracy, speed, and accessibility of symptom analysis.
AI’s Contributions to Symptom Evaluation
| Feature | AI Application |
| Natural Language Processing | Interprets typed or spoken symptoms |
| Predictive Modeling | Assesses symptom clusters to predict conditions |
| Clinical Decision Support | Recommends next diagnostic steps |
| Patient Chatbots | Provide 24/7 guidance based on symptom inputs |
Real-World Example
A study published in The Lancet Digital Health (2022) found that AI symptom checkers correctly triaged 85% of patients in simulated emergencies — a promising indicator of how tech is reshaping healthcare.
How to Perform a Self-Symptom Analysis Safely
While online tools can help, self-analysis should be approached cautiously.
Steps for Self-Evaluation
- Log symptoms consistently: Time, triggers, duration, and severity
- Use credible online resources: Mayo Clinic, NHS, MedlinePlus
- Recognize red flags: Severe, sudden, or worsening symptoms need medical attention
- Avoid self-diagnosing complex conditions
Red Flag Symptoms That Require Immediate Care
| Symptom | Possible Indication |
| Sudden chest tightness | Myocardial infarction |
| Slurred speech or weakness | Stroke |
| High fever with rash | Sepsis, meningitis |
| Difficulty breathing | Asthma attack, PE, pneumonia |
| Severe abdominal pain | Appendicitis, bowel obstruction |
Symptom Patterns Across Common Diseases
Recognizing symptom clusters is key to identifying the most likely cause.
Examples of Symptom Patterns
COVID-19
- Fever
- Dry cough
- Fatigue
- Loss of taste/smell
Depression
- Low mood
- Loss of interest
- Insomnia or hypersomnia
- Fatigue
Type 2 Diabetes
- Frequent urination
- Excessive thirst
- Blurred vision
- Slow wound healing
Irritable Bowel Syndrome (IBS)
- Bloating
- Abdominal pain
- Alternating constipation and diarrhea
Learning these clusters allows quicker recognition and action, both in clinics and at home.
Symptom Analysis vs. Diagnosis
Let’s clarify a common misconception.
| Aspect | Symptom Analysis | Diagnosis |
| Objective | Understand what the patient feels | Name the underlying condition |
| Based on | Symptoms and patterns | Analysis, tests, history |
| Who performs it | Patient or professional | Qualified medical practitioner |
| Outcome | Preliminary insights | Official medical classification |
Diagnosis is the final result of several processes — symptom analysis is where it all begins.
Symptom Tracking and Journaling
Why Track Symptoms?
Tracking your symptoms over time is one of the best ways to understand patterns, triggers, and severity. Whether you’re managing a chronic condition or trying to figure out the root cause of sudden changes in health, symptom tracking provides a valuable record to share with healthcare providers.
Benefits of Symptom Journaling:
- Increased diagnostic accuracy: Helps identify consistent patterns.
- Improved treatment planning: Helps doctors prescribe appropriate treatments and adjustments.
- Encourages proactive health management: Patients can take charge of their well-being.
How to Track Symptoms Effectively
- Use an app or physical journal: Record the time, intensity, and duration of each symptom.
- Note any triggers or changes: Food, stress, environment, or physical activity can all impact symptoms.
- Share your journal with a healthcare provider: A comprehensive record can improve decision-making and lead to faster diagnosis.
Case Study: Symptom Analysis in Chronic Illness
Chronic Fatigue Syndrome (CFS)
Patient Background: Sarah, a 38-year-old woman, has been experiencing persistent fatigue, joint pain, and trouble concentrating for over six months.
Symptom Analysis:
- Duration: Fatigue lasting for more than 6 months
- Provocation/Palliation: Worsens after physical or mental activity, slightly relieved by rest
- Severity: 8/10
- Onset: Gradual onset after a viral infection
Outcome: Through detailed symptom analysis, her doctor was able to diagnose Chronic Fatigue Syndrome. While it took time, the consistent tracking of symptoms allowed Sarah’s doctor to rule out other conditions and provide a treatment plan tailored to her unique symptoms.
User Behavior and Bias in Symptom Reporting
Patients’ subjective reports of symptoms may be influenced by biases and psychological factors that can cloud the diagnostic process. These include:
- Health anxiety: Some individuals may exaggerate symptoms due to anxiety, leading to unnecessary concern.
- Cultural factors: Different cultures may interpret or describe symptoms differently.
- Gender bias: Certain symptoms in women (e.g., chest pain) may not be taken as seriously as in men.
Understanding these biases and reporting accurately is essential for a successful analysis.
Future Trends in Symptom Analysis
As technology advances, so will the methods we use to analyze symptoms.
- AI and machine learning: AI models will increasingly use vast databases of symptoms to predict diagnoses.
- Wearable health technology: Devices will continue to track real-time data,
including vital signs and physical activity, which can be integrated into symptom analysis.
Conclusion: Empowering Health Through Symptom Awareness
Symptom analysis is a cornerstone of healthcare. By recognizing patterns, using technology, and tracking symptoms accurately, individuals and healthcare providers can work together to uncover the root causes of health issues. Whether you’re managing a chronic illness or simply trying to stay on top of your health, understanding your symptoms is the first step toward better health outcomes.


 Prevention Is the New Cure
Prevention Is the New Cure What Does It Mean to Predict Disease?
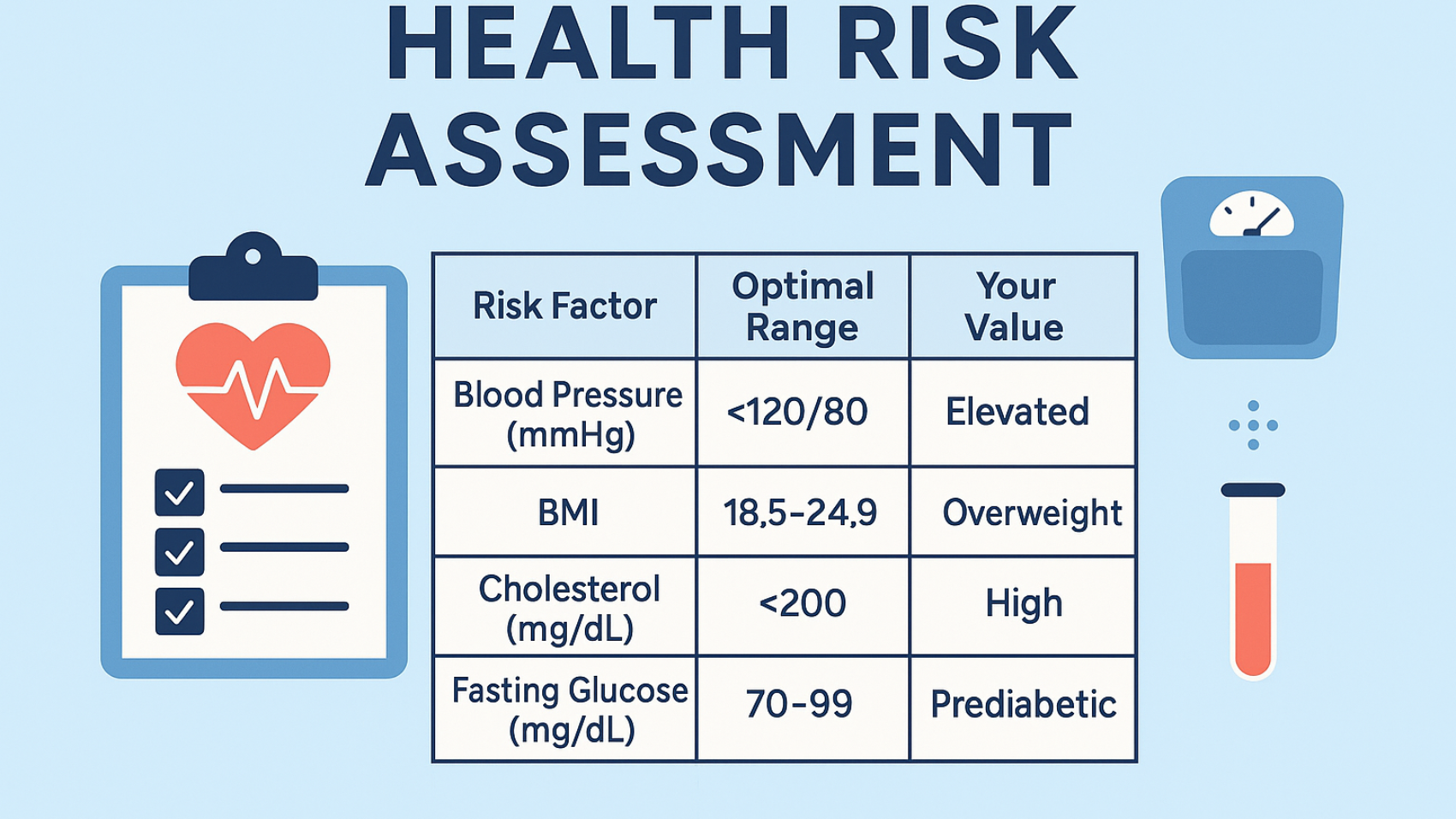
What Does It Mean to Predict Disease? Table: Common Diseases and Early Predictive Indicators
Table: Common Diseases and Early Predictive Indicators Why Predicting Disease Early Is Critical
Why Predicting Disease Early Is Critical Faster intervention – Catch issues early and reverse them before they worsen
Faster intervention – Catch issues early and reverse them before they worsen Lower healthcare costs – Prevention is cheaper than treatment
Lower healthcare costs – Prevention is cheaper than treatment Improved quality of life – Live symptom-free and stay productive
Improved quality of life – Live symptom-free and stay productive Reduces risk of complications – Especially for chronic conditions like diabetes and hypertension
Reduces risk of complications – Especially for chronic conditions like diabetes and hypertension Tools That Help Predict Potential Health Issues
Tools That Help Predict Potential Health Issues Use it as your go-to tool to spot red flags and make smarter health choices.
Use it as your go-to tool to spot red flags and make smarter health choices. Chart: Health Data from Wearables Over 30 Days
Chart: Health Data from Wearables Over 30 Days Observation: Gradual increases in resting HR and decreases in SpO₂ & sleep time could indicate rising cardiovascular or respiratory risk.
Observation: Gradual increases in resting HR and decreases in SpO₂ & sleep time could indicate rising cardiovascular or respiratory risk. Tip: Combine genetic data with test results on Health Audit X for smarter predictions.
Tip: Combine genetic data with test results on Health Audit X for smarter predictions. How to Predict Chronic Health Issues at Home (Step-by-Step)
How to Predict Chronic Health Issues at Home (Step-by-Step) Step 1: Track Basic Health Metrics
Step 1: Track Basic Health Metrics Predictive Health in Action: Real-World Case
Predictive Health in Action: Real-World Case Prevention in action!
Prevention in action! Tips to Prevent Predictable Diseases
Tips to Prevent Predictable Diseases Eat for Prevention
Eat for Prevention Move Daily
Move Daily Sleep Well
Sleep Well Manage Stress
Manage Stress How Health Audit X Makes Predicting Disease Easy
How Health Audit X Makes Predicting Disease Easy
 Upload & analyze lab reports
Upload & analyze lab reports AI-powered predictions
AI-powered predictions Compare the values with normal ranges
Compare the values with normal ranges Risk levels (Low, Moderate, High)
Risk levels (Low, Moderate, High) Routine tracker for vitals, meals, and symptoms
Routine tracker for vitals, meals, and symptoms Your data is private, secure, and used only to help you stay healthy.
Your data is private, secure, and used only to help you stay healthy. The Future of Predictive Healthcare
The Future of Predictive Healthcare Final Thoughts: Predict, Prevent, Protect
Final Thoughts: Predict, Prevent, Protect Start now:
Start now: Your health is in your hands—make it a priority.
Your health is in your hands—make it a priority.